Maternal and Child Health
Maternal and infant mortality in India remains unacceptably high. This part of the booklet aims to allay the anxiety and fears of young mothers who are worried about pregnancy, delivery, and the subsequent care of their newborn. Most of these fears arise due to ignorance about some basic aspects of care during pregnancy and care of the infant. We can avoid many maternal and infant deaths if we take just a few basic precautions in the care of mothers and children.
Antenatal care (care during pregnancy) To ensure the good health of a mother and her child, it must be understood that the care of a newborn starts even before the child is born. This means that every pregnant woman must take good care of herself by following certain simple rules:
To ensure the good health of a mother and her child, it must be understood that the care of a newborn starts even before the child is born. This means that every pregnant woman must take good care of herself by following certain simple rules:
- As soon as you know that you are pregnant, get yourself registered at the earliest in an antenatal clinic (ANC) in a nearby hospital, dispensary, health centre, or sub-centre.
- Attend this clinic as advised by your health professional. You must go for at least 3 checkups in this ANC: first at the time of registration, second at 24 – 28 weeks, and third at 3 – 4 weeks before the expected date of delivery. During these visits you will be examined for your height and weight, your blood pressure will be taken, and certain necessary investigations, e.g., a haemoglobin test and urine examination, will also be carried out.
- High-risk mothers need to visit the ANC more frequently, as chances of problems arising during pregnancy are greater. You are a ‘high-risk mother’ if you have even one of the following:
- Age less than 18 years or more than 35 years
 Height 140 cm or less
Height 140 cm or less- Bleeding through vagina or pain in abdomen during pregnancy (indicating threatened miscarriage)
- Anaemia (lack of iron), swelling of feet, high blood pressure (BP) and protein in urine during pregnancy (pre-eclampsia), or convulsions (eclampsia)
- Are pregnant with twins
- Have a history of caesarean operation or forceps delivery
- Malpresentation (the fetus is not in the head-down position by the last month of the pregnancy)
- Have a disease, e.g., heart disease, high BP, kidney disease, diabetes, tuberculosis or liver disease
- Are over 30 years old and are pregnant for the first time
- You must take injections of tetanus toxoid (TT) during pregnancy. If this is your first pregnancy, take 2 injections of TT with a gap of 4 – 6 weeks between them. These injections can be taken any time during pregnancy and are essential to protect you and your child against a deadly disease called tetanus.
- If this is your second pregnancy and it has occurred within 3 years of your first pregnancy, you need to take only 1 injection of TT provided you have taken 2 injections of TT during the first pregnancy. If not, you need to take 2 injections.
- Take folic acid tablets for the first three months and iron, folic acid and calcium tablets thereafter to prevent anaemia during pregnancy. (Remember, if you already suffer from anaemia, you will require two tablets of iron and folic acid.)
- Take rest, sleep eight hours at night and, if possible, two hours in the afternoon.
- Do not smoke or drink. Also make sure that others do not smoke in your vicinity.
- Do not take any medicine unless prescribed by a qualified doctor. Similarly do not get investigations like x-rays and ultrasound done on your own. Both of these can be harmful.
- Keep yourself neat and clean.
- Keep your breasts clean; wash them daily. If the nipples of your breasts are inverted (pointing inwards), this is the time to deal with this problem. Try to gently pull them out and hold them in this position for a few minutes. This can be repeated 5 – 6 times daily.
- If possible, sexual intercourse is better avoided in the first three months and last six weeks of pregnancy.
- Look out for any of these symptoms. These are danger signals and need immediate attention from a health professional:
- Persistent headache
- Reduction/blurring of vision
- Swelling around your ankles
- Pain in your abdomen
- Bleeding, spotting, or excessive and watery vaginal discharge
- Make plans for the delivery of your child a few weeks before the expected date of birth. It is important that your delivery is conducted by a trained health professional in a clean and safe environment.
- It is also important to find out about the nearest hospital, where you can be taken in case there is a problem during delivery. Also do not forget to arrange for a vehicle to be available in advance.
- Eat a balanced and nutritious diet. Compared to your pre-pregnancy state, you require at least 50% more food during your pregnancy. Remember, if you eat well, the baby inside ‘eats’ well and will be born with a good birth weight. Include lots of green leafy vegetables for iron, fresh seasonal fruits for vitamins, jaggery for energy, and gram (chana), peas and pulses for proteins – the body-building nutrients in your diet. If possible, take at least two glasses (total 500 mL) of milk everyday.
Iron Content in Food
| High: More than 5 mg/100g | |
|---|---|
| Whole wheat flour | Turnip leaves |
| Wheat germ | Onion stocks |
| Dalia | Plantain green |
| Rice flakes | Lotus stem |
| Bajra | Watermelon |
| Peas dry | Almonds |
| Soyabean | Raisins |
| Rajmah | Gingelly seeds |
| Lobhia | Nigella seeds |
| Lentil | Tamarind pulp |
| Bengal Gram Dal | Coriander seeds |
| Bengal Gram, whole | Zeera |
| Bengal Gram, roasted | Ajwain |
| Bengal gram leaves | Mango Powder |
| Colacasia leaves | Turmeric powder |
| Cauliflower leaves | Munakka |
| Mustard leaves | Jaggery |
| Table Radish Leaves | |
| Low: Less than 5 mg/100g | |
|---|---|
| Jowar | Peas, green |
| Maize | Bathua leaves |
| Barley | Sem beans |
| Rice | Apple |
| Ragi | Amla |
| Spinach | Cashew Nuts |
| Methi | Sapota |
| Amaranth | |
Natal care (during childbirth)
Place of delivery
- If possible the first delivery should take place at a hospital.
- In case of home delivery, it should be by a trained birth attendant/health professional. The room should be warm, clean and well ventilated, with adequate light. Put the bed or mat and blankets in the hot sun before use.
- To maintain clean hands, the birth attendant should cut her nails and wash her hands well with soap and water before conducting the delivery. She should not wipe her hands or touch anything.
- Perform the delivery on a clean surface or clean bed sheet.
- Use clean thread for tying the umbilical cord.
- Use a new, clean blade for cutting the cord.
- Do not apply anything on the cord. Keep the cord clean.
- Inform the dai, auxiliary nurse midwife (ANM), or nurse as the case may be.
- Keep ready a new blade, soap, thread or cord tie and gloves (the disposable dai kit), and a clean cloth for wrapping the baby, sanitary napkins for the mother, cotton gauze, and boiled water.
- Take plenty of liquids during labour pain.
- Walk in early stages of labour.
- Lie down on a bed and take deep breaths after the bag of water breaks.
- Do not press the abdomen from the outside and do not lie on your stomach.
- Do not break the water bag with a nail or blade.
- Do not take any injections to speed up the delivery.
- Do not push the baby down in between pains.
- Do not pull the baby out by force.
- Do not do frequent vaginal examinations.
- Wipe the baby clean with a soft, clean cloth at birth.
- Wrap the baby in two layers of clothes. Keep the baby by the side of the mother as her body temperature will keep the baby warm.
- Start breastfeeding within a half hour after delivery. Ensure that the baby is not exposed to a direct draught of air. Do not give a low-birth-weight baby (less than 2.5 kg) a bath for one week after birth.
- Ensure the baby is handled by only one or two persons.
The mother and/or baby should be shifted to a hospital immediately if any of these danger signs appear:
- There is excessive vaginal bleeding before or after the baby is delivered.
- The mother is in labour for 24 hours without delivering the baby.
- The baby’s hand or foot comes out first.
- There is dirty-looking discharge.
- The mother has fits during delivery.
- The mother has severe pains in the abdomen or severe paleness or breathlessness.
- The baby appears pale, blue or does not cry.
- Nutritious food is a must for the mother after childbirth.
- Continue taking iron, calcium and a high protein diet.
- Drink plenty of liquids, including milk.
- Vaccinate the child as required.
- Exclusively breastfeed till 6 months. Clean your nipples and areola before breastfeeding the child.
- Take a daily bath and change pads every 6 – 8 hours.
- A minimum of three postnatal visits by a dai or nurse or in a hospital within six weeks after delivery are a must.
- High-grade fever or foul-smelling vaginal discharge after delivery or up to 40 days after childbirth
- Excessive vaginal bleeding within 40 days after delivery
- Headache and vomiting or fits
- Severe pain in the abdomen within 40 days
Care of the newborn starts with good antenatal care, safe delivery at a hospital or by a trained birth attendant at home, and includes:
- Resuscitation at birth if necessary
- Management of hypothermia (below normal temperature)
- Prevention of infections
- Care of low-birth-weight (less than 2.5 kg) babies
- Identification of high-risk newborns
- 95% of newborns cry immediately after birth. The colour of their skin is pink and they breathe easily. Their heart rate is approximately 120 – 160 per minute. Such newborns should be wiped with a soft clean cotton cloth and wrapped in warm clothes and kept near their mother for breastfeeding.
- Some newborns do not cry at birth and breathe irregularly. Their skin colour is blue or pale, and their heart rate is also less than 100 per minute or is not at all audible. These are signs of birth asphyxia.
- Put the child under a warmer or bulb if possible.
- Place the child on its side so that fluid can come out easily.
- Suck out aspirated fluids with a mucus extractor if possible. Clean the baby’s mouth, nose and throat so that airways are not blocked.
- Respiration is stimulated with cleaning of airways and most newborns start crying thereafter. If not, stimulate the soles of the feet with your fingers, or the baby’s back can be rubbed softly.
- Mouth-to-mouth respiration should be given. Blow with the cheeks rather than full breaths as a baby’s lungs are very small and delicate.
- Take the newborn to the hospital immediately if the above measures fail.
- Don’t keep the child upside down.
- Don’t place the baby face down.
- Don’t pat the baby hard on the back.
- Don’t press the baby’s abdomen.
- Don’t sprinkle hot or cold water on the baby.
 In hypothermia, a newborn loses heat from all parts of his body and is unable to generate heat to maintain its body temperature. Temperature falls very quickly if not properly maintained, which can be fatal. Low temperature can be assessed by recording axillary (under the arm) temperature. (Normal is 98.4˚ F.)
In hypothermia, a newborn loses heat from all parts of his body and is unable to generate heat to maintain its body temperature. Temperature falls very quickly if not properly maintained, which can be fatal. Low temperature can be assessed by recording axillary (under the arm) temperature. (Normal is 98.4˚ F.)
If palms and soles are cold, but chest and abdomen are warm.
HypothermiaIf all parts are cold. A normal newborn is warm to the touch and its colour is pink.
Prevention of hypothermia- Wipe the newborn with a clean warm towel immediately after birth.
- Then wrap the baby in another warm dry towel or with cotton from head to foot.
- The newborn should be kept next to the mother’s skin.
- The room should be warm; fans should be switched off.
- Put the newborn under a warmer if one is available, or 1½ feet away from a 200-watt bulb. Keep the room warm with a heater or a hot water bottle.
- Put the child between the mother’s breasts (kangaroo method).
A newborn is prone to infections, which are a major cause of death.
- Take two injections of tetanus toxoid during each pregnancy.
- Choose a delivery place that is clean, airy and well-lit.
- Make sure the birth attendant should washes her hands thoroughly with soap and water before conducting the delivery.
- Cut with a clean new blade, tied with sterilized cord ties and left dry and clean. The care of the cord is important.
- Ensure that any person who has to hold the newborn washes his/her hands thoroughly for one minute before touching the baby.
- Cut the baby’s nails cut clean.
- Continue Breastfeeding for six months.
- Use clean clothes for the newborn.
- Get the child immunized.
- Don’t give the child honey, tea, gur, water or ghutti or bottlefeed.
- Don’t let a sick person hold or attend to the newborn.
- Don’t take a newborn to a crowded place.
- Don’t allow many persons to enter the room where the newborn is lying.
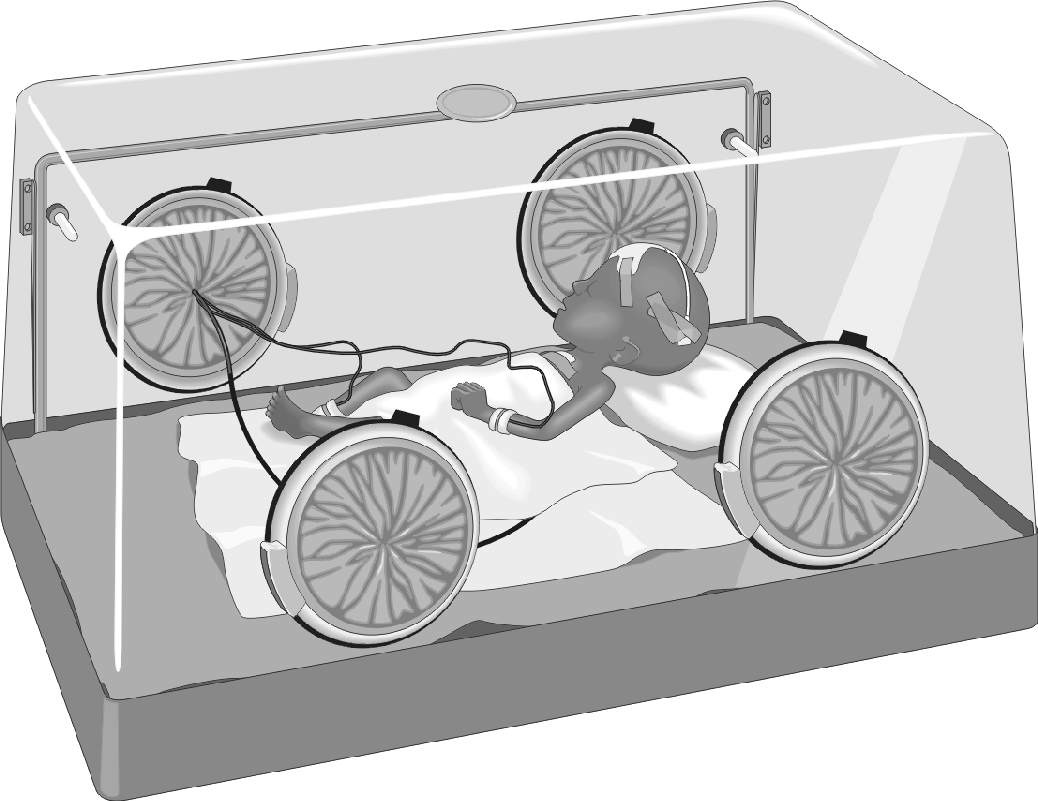
The normal birth weight of a newborn is 2.5 kg. If a newborn weighs less than 2½ kg, it is known as a low-birth-weight baby. Newborn babies whose weight is between 2.0 and 2.5 kg can be managed at home. Babies who weigh less than 2 kg may have to be kept at a hospital.
Home management of babies with low birth weight- During the first week, sponge-bathe the newborn daily. At the end of the first week, bathe the newborn.
- Managing hypothermia is important. Keep the newborn wrapped in woolens or next to the mother’s skin. ‘Kangarooing’ should be done by keeping the child between the mother’s breasts.
- Keep the baby in a clean and airy room; the room should be kept cosy.
- Exclusive breastfeeding should be practiced. Feed the baby frequently, every two hours at least, as it gets tired easily and may feed only for a short time.
- If a baby is unable to suck, express breast milk into the baby’s mouth or into a bowl and feed with a spoon.
- Watch for diarrhoea and acute respiratory infections. If there is diarrhoea, give ORS (oral rehydration solution) and take the baby immediately to a doctor.
- Immunization is very important as a weak child is prone to infections.
- The child should be handled by as few people as possible. Sick persons should not go near the child.
The future mother should:
- Start taking iron tablets after 12 years of age.
- Avoid pregnancy before 21 years of age.
- Take one extra meal and avoid very hard work during pregnancy.
- Avoid smoking and alcohol completely.
- Rest for at least 2 hours in a lying down position during the day and get adequate sleep of 8 hours at night during pregnancy.
- Take folic acid tablets for the first three months and iron, folic acid and calcium tablets thereafter during pregnancy.
- Get at least three antenatal checkups by doctors.
- Detect any anaemia, high blood pressure and bleeding early for referral to hospital.
- Space births at least 3 years apart.
Arrange to take the newborn to a hospital if:
- Birth weight is less than 1800 g or there was a premature delivery (baby was born before the due date).
 Breathing is difficult or laboured.
Breathing is difficult or laboured.- Child is unable to suck or breastfeed.
- Child is having fits or convulsions.
- Child is sleepy or cries a lot.
- Child is pale.
- Child has fever or is cold.
- Child is bleeding from any site.
- Abdomen is distended (swollen) or child is vomiting.
- There is pus from the cord.
- Child has any birth defects.
- Breast milk is a balanced meal for the first six months of life. First milk (colostrum) should always be given to the newborn. This acts to boost the immune system and to protect the newborn from infection. It acts as its first immunization.
- Breastfeeding should be started between half an hour and two hours after delivery or as early as possible.
- Feeding should be every two hours or feed on demand.
- Exclusive breastfeeding should be done for the first six months.
- Don’t give water, ghutti, or bottle feed.
- When the infant is six months old, start weaning with liquid foods like daal ka paani, rice water, and lassi. Then give semi-solid foods like dalia, khichdi, suji ki kheer, boiled and mashed potatoes, mashed banana, and homemade cerelac. Continue breastfeeding.
- Give the above three to four times a day initially.
- Then increase the quantity and give food more frequently.
- At nine months give everything that is cooked for adults.
- At 1½ years of age, the child should eat half of what an adult eats.
Look for the following signs in the newborn:
- The child is cold or has high fever with chills.
- Breathing is fast and laboured.
- The child is unable to suck or eat food.
- The child is abnormally sleepy or difficult to awaken.
- There is indrawing of the chest when the child is calm. (A deep groove appears between the chest and tummy when the child breathes in.)
- When the child is calm, there are wheezing noises in the chest.
- Give plenty of liquids.
- Continue breastfeeding.
- Keep child warm.
- Keep the child in clean, non-smoky air.
- Immediately take the child to the doctor or hospital if you see any of the above problems.
- Do not give home remedies if any of the above problems are present.
- Do not go to ‘roadside doctors’ (quacks) for treatment.
 It is absolutely essential to protect the child against deadly diseases like tuberculosis, diphtheria, whooping cough, tetanus, polio, measles and hepatitis B. A child who is not immunized is likely to become disabled or undernourished and may die.
It is absolutely essential to protect the child against deadly diseases like tuberculosis, diphtheria, whooping cough, tetanus, polio, measles and hepatitis B. A child who is not immunized is likely to become disabled or undernourished and may die.
Immunization schedule
| 1. | At birth | BCG/OPV zero dose |
| 2. | 1½ months | DPT and OPV 1st dose + Hepatitis B 1st dose |
| 3. | 2½ months | DPT and OPV 2nd dose + Hepatitis B 2nd dose |
| 4. | 3½ months | Hepatitis B 3rd dose |
| 5. | 9 months | Measles and Vit A 1st dose |
| 6. | 16 – 24 months | DPT and OPV booster + Vit A 2nd dose |
| 7. | 2 years | Vit A 3rd dose |
| 8. | 2½ years | Vit A 4th dose |
| 9. | 3 years | Vit A 5th dose |
| 10. | 4½ to 5 years | DT and OPV booster + Hepatitis B booster |
| 11. | 10 & 16 years | T-T + Hepatitis B booster |
- All children 0 – 5 years of age should be given 2 drops of OPV during pulse polio program.
- Immunization is urgent and has to be done in the first year of life.
- Diarrhoea can kill a child quickly by loss of liquid from the body.
- Give plenty of liquids to the child, like coconut water, shikanji (lemon water), light tea, lassi (buttermilk), soup, khichdi, light daal, dalia, good cooked rice, and boiled and mashed potato (if the child is not still breastfeeding).
- Give ORS (oral rehydration solution) or jeevan rak-shak ghol.
- Continue breastfeeding.
- Consult a doctor if diarrhoea is present for several days or there is blood in the baby’s stools.
- Give a child who has recovered from diarrhoea at least one extra meal each day for at least two weeks.

- The child has uncontrolled vomiting and diarrhoea.
- There is blood in the stool.
- The child is not taking fluid or food orally.
- The child is sleepy and difficult to awaken.
- The child faints due to dehydration.
- Weak crying, no tears from the eyes, dry mouth and lips
- Loss of skin elasticity
- Sunken eyes and sunken fontanel (soft areas in the child’s skull)
- Decrease in amount of urine
- Breastfeed exclusively: no ghutti or bottle for the first six months of life.
- Keep food and water for drinking covered and away from flies.
- Keep child clean, cutting nails regularly.
- Wash hands with soap and water before taking food and after using the toilet.
Malnutrition
Causes of malnutrition- Weaning done early, not at proper age (seventh month)
- Poor hygiene/poor diet
- Worm infestation
- Repeated episodes of diarrhoea/chest infection
- Child not gaining weight and attaining required height
- Weight for age in growth chart is low
- Generalized swelling of the body or very thin body
- Repeated skin infections like boils
- History of eating inedible things like soil, chalk, paper, pencils, hair, etc.
- Diet rich in proteins
- Treatment for worm infestations
- Nutritional recipes like homemade cerelac:
- Use 250 gms roasted channa + 100 gms of murmura.
- Grind separately and sieve.
- Mix and keep in airtight container.
- Mix 4 spoons in a bowl of milk with sugar for each feeding.
- Age at marriage should be more than 18 years.
- Bearing a child before 21 years can be dangerous for the life of both mother and child.
- All adolescent girls (10 – 14 years) should take one tablet of iron every alternate day for prevention of anaemia.
- Iron prevents anaemia and thus helps prevent the problem of low birth weight if it is given till the girl gets married and conceives. Iron should be given as per the same schedule (three times a week) to newlywed women also, till they miss their menstrual period and pregnancy is confirmed.
- Anaemia can be prevented by a diet rich in iron. Eat saag, palak, chaulai, methi, mooli, sprouted daals, and gur.
- Cooking in iron utensils is also useful.
- Maintenance of hygiene is important during menstruation; use of sanitary napkins is a must for the prevention of reproductive tract infections.