Eye Care
Eyes are the windows to the outside world. They are nature’s priceless gift. We can realize just a bit of the plight of a blind person if we close our eyes and try to move around.
Our eyes take care of us throughout our life. Likewise, we must take care of them. Eye problems can occur at any stage of human life. Certain eye diseases occur while the baby is still in the mother’s womb. Others present themselves when the child is born. There are eye conditions that are predominantly encountered during a child’s growing years (pre-school and school-going age). People are faced with a variety of eye problems during young adulthood, middle age, elderly years and extreme old age.
 One important fact to be remembered is that many eye problems, if not recognized and treated in time, can lead to blindness. A second important fact is that many of these blinding conditions are preventable. Preventing a disease is more effective, convenient, cheaper and much easier than getting a disease and having to treat it.
One important fact to be remembered is that many eye problems, if not recognized and treated in time, can lead to blindness. A second important fact is that many of these blinding conditions are preventable. Preventing a disease is more effective, convenient, cheaper and much easier than getting a disease and having to treat it.
Now let us see how care of the eyes is required right from the beginning of life in the mother’s womb, and should be continued till the end of your life and even thereafter (for eye donation).
Care of the baby’s eyes in the mother’s wombDuring pregnancy (the antenatal period) poor nutrition, anaemia, medications containing steroids, x-ray examination of the abdomen and rubella (German Measles) infection can harm the eyes of an unborn baby by causing blindness due to conditions such as congenital cataract, glaucoma and retinopathy. To prevent such complications, you should:
- Vaccinate girls against rubella (MMR) before puberty
- Avoid unnecessary abdominal x-rays and steroid intake
- Ensure proper nutrition
- Avoid unnecessary drugs during the first three months of pregnancy
 A baby’s face, especially the area around the eyes, should be cleaned with a sterile lint before opening them. Thereafter antibiotic drops need to be instilled into the eyes of the baby. If there is any watering or discharge from the baby’s eyes during the first month of life, you must consult your eye doctor without delay. Such a condition may be simple conjunctivitis (eye flu), but it may be one of the following serious conditions:
A baby’s face, especially the area around the eyes, should be cleaned with a sterile lint before opening them. Thereafter antibiotic drops need to be instilled into the eyes of the baby. If there is any watering or discharge from the baby’s eyes during the first month of life, you must consult your eye doctor without delay. Such a condition may be simple conjunctivitis (eye flu), but it may be one of the following serious conditions:
- Ophthalmia neonatorum (eye infection of the newborn)
- Congenital glaucoma (baby has high pressure in the eyes)
- Nasolacrimal-duct block (blockage of tear outflow channels)
In such conditions, follow the treatment advised, and you will save the child from vision loss and other eye complications. If the pupil of the baby’s eye has a white discoloration, it may be due to a congenital cataract or cancer of the eye (retinoblastoma) or another serious eye condition. Consult your eye doctor.
Eye problems in growing childrenAs the baby grows, the following eye problems may be encountered:
Nutritional blindnessVitamin A deficiency in children can cause night blindness, dryness of the eye (xerosis), keratomalacia (ulcerations and dissolution of cornea, which is the front transparent covering of eye) leading to total blindness and even loss of an eye. This condition is known as nutritional blindness. It commonly affects children below five years of age especially if they suffer from protein-calorie-malnutrition. Additional factors include URI (upper respiratory tract infection), measles, diarrhoea and worm infestation.
Prevent nutritional blindness by eating
carrots, mangoes, papayas, dark green leafy vegetables
(like palak and bathua), and milk-based foods.
Give breast milk to newborns and infants.
If you cannot get these foods, then give children (between the age of six months and six years) doses of vitamin A every six months.
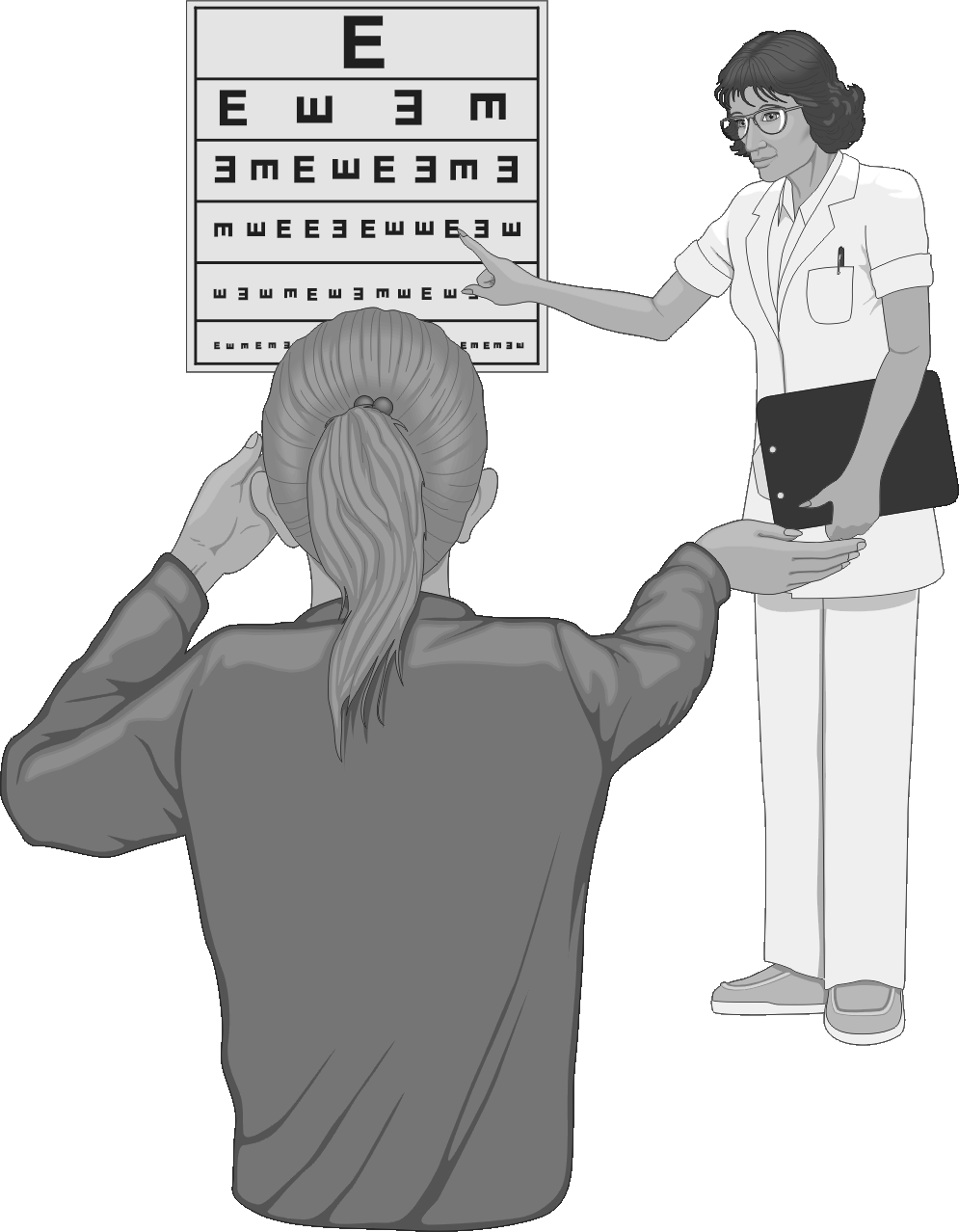
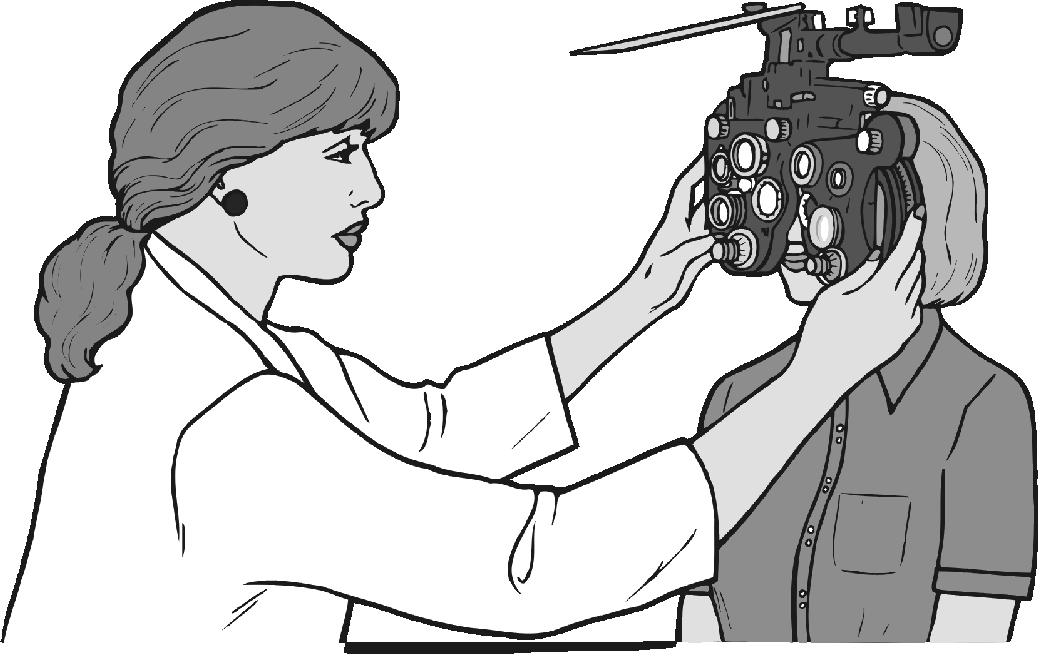
Eye problems in school-going children from 6 to 14 yearsThere should be a check-up for refractive errors (near-sightedness, far-sightedness, and astigmatism), amblyopia (lazy eye), squint and colour vision defects.
Refractive errors (problems needing spectacles) In this group there are three main conditions that cause poor vision and sometimes blindness. These are:
In this group there are three main conditions that cause poor vision and sometimes blindness. These are:
- Short-sightedness or near-sightedness (myopia)
- Far-sightedness (hypermetropia)
- Astigmatism (uneven curvature of the surface of the eye)
All the three problems happen to people of all ages and they can usually be helped by wearing spectacles. Short- and far-sightedness are caused by a change in the shape of the eyeball. In children, these problems are congenital. If children have one of these problems, they will:
- Blink frequently and rub their eyes
- Squeeze or narrow their eyes to see a distant or close object
- Hold a book close to the eye
- Not be able to read a clock at a distance
- Often stumble, particularly in dim light
- Lose interest in activities around them
Children usually don’t say they have poor vision. They may not even notice their problem and may adjust to their poor eyesight by sitting near the television or blackboard or by squeezing their eyes.
Check your children’s eyesight before
they start school and later also at least once or twice
during their school years (between 6-14 years)
for early diagnosis and treatment of problems.
Deviated eye (squint) is not only a cosmetic problem but it can also cause blindness (amblyopia). Get it corrected as soon as possible.
Colour vision defectsThese defects are often detected at the time of selection of a child for a particular career. At this stage, the child may be rejected because of defective colour vision and feels very much disheartened. If the colour vision defect is detected early, this may help the child and the parent to make up their mind for a career where colour vision is not really important.
InjuriesInjuries to the eyes may cause blindness. Children are prone to injuries. Eye injuries are commonly caused by:
- A direct hit on the eye (e.g., by a ball or a blunt object)
- Sharp objects entering the eye
- Chemicals entering the eye
- Heat injuries (burns)
- Gunshot and landmine injuries
- Head injuries (a serious hit on the head)
- Road accidents
- Take care when children play games like gullidanda and bows and arrows.
- Do not let children play with sharp-edged toys, knives, scissors, needles or any other sharp objects.
- Do not let children play with firecrackers
- Do not look at the sun directly with or without dark glasses, particularly during a solar eclipse. The sun can burn the retina, which is very delicate. This can damage the eyesight or cause blindness.
- If you are a bus driver, truck driver or you drive any type of vehicle, have your eyes tested every year. Never drink alcohol before or while driving.
- Wear protective (safety) glasses when working with chisels, saws or other machinery, and particularly when welding.
 Trachoma is an infection of the eye caused by a germ called Chlamydia trachomatis. Left untreated, it can lead to blindness. It is common in India, especially in villages among people living in unhygienic conditions. Trachoma occurs when:
Trachoma is an infection of the eye caused by a germ called Chlamydia trachomatis. Left untreated, it can lead to blindness. It is common in India, especially in villages among people living in unhygienic conditions. Trachoma occurs when:
- Too many people are living together.
- There is no clean water.
- There is an increased number of eye-seeking flies. (In India this happens in April-May and during July-September when high temperature and rainfall favour the increase in fly population.)
- You share towels, handkerchiefs and pillows, etc.
- You apply kajal or surma with a shared rod.
- You live in a dry and dusty environment.
- There are conditions of poverty, ignorance, poor personal hygiene, and lack of knowledge about spread of contagious disease. As living conditions improve, the disease tends to regress.
Trachoma infection by itself (“pure” trachoma) is a relatively mild condition, so mild and symptomless indeed as to excite little or no attention. However, in the absence of treatment, the disease runs a persistent course (subacute trachoma) and ultimately leads to opacity of the transparent covering of the eye (cornea) leading to blindness. The cornea becomes opaque in the following ways:
- There is roughening and scarring of the undersurfaces of the eyelids (hallmark of trachoma) with inturning of eyelashes (trichiasis). The uneven undersurface of the eyelids and misdirected eyelashes rub the cornea with every blink and damage it, finally making it opaque due to scarring.
- Trachoma germs can cause an ulcer on the cornea directly which, when healed, leads to opacity.
- Eyes with trachoma are vulnerable to secondary infection with other types of germs (previously known as “acute” trachoma) resulting in an acute and severe ulcerative condition of the cornea. These are liable to relapse and lead to more scarring, more opacity and blindness.
TO PREVENT TRACHOMA:
Wash your eyes with clean water.
Keep yourself and your surroundings clean.
IF YOU HAVE AN EYE INFECTION:
Show it to a qualified doctor.
Use the right medicines (antibiotics) early.
Follow the SAFE strategy as recommended by WHO (the World Health Organization). The components of the SAFE strategy are:
- S –
- Surgery to correct trichiasis (inturned eye lashes),the immediate precursor to blindness
- A –
- Antibiotics to treat an active disease (as advised by an eye specialist)
- F –
- Facial cleanliness to reduce transmission of infection
- E –
- Environmental improvement (clean latrines, fly control, clean water supply, proper garbage disposal, etc.)
A corneal ulcer is a discontinuity in the surface cells of the cornea (the cornea is the frontmost clear layer of the eye that allows light to enter). A corneal ulcer is a sight-threatening condition.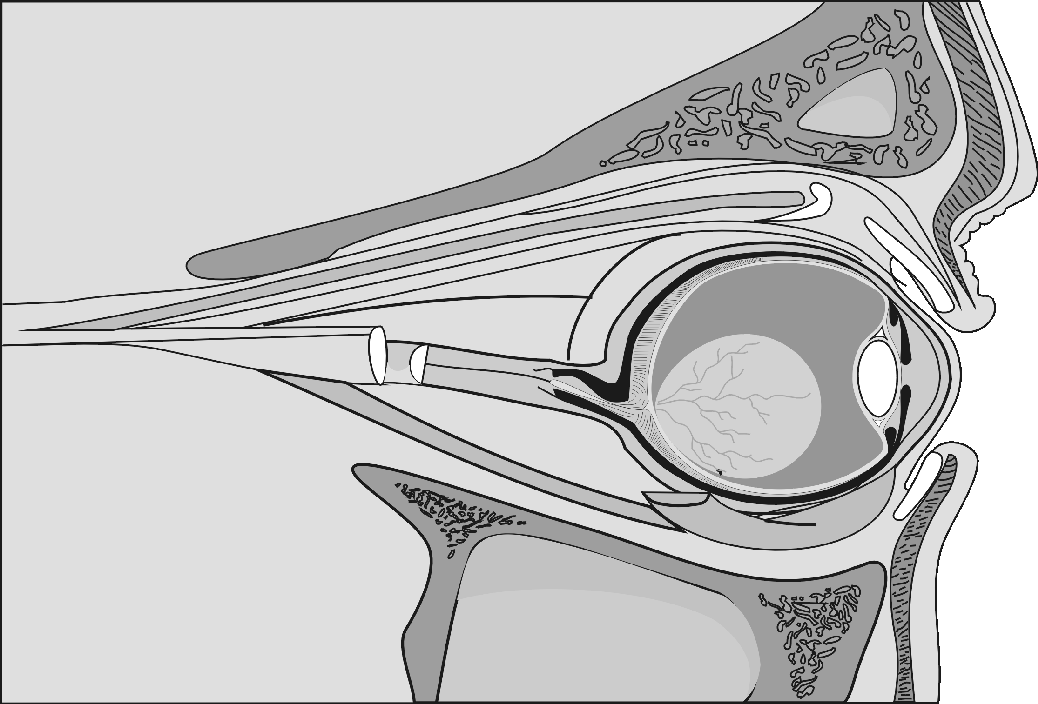 It usually occurs due to abrasions or scratches on the corneal surface that get infected with bacteria, fungus, or virus. These scratches or abrasions result from trivial injuries and foreign bodies. Certain eye conditions like misdirected eyelashes (trichiasis) and granular deposits (concretions) on the under-surface of the eyelids can also scratch the cornea with every blink.
It usually occurs due to abrasions or scratches on the corneal surface that get infected with bacteria, fungus, or virus. These scratches or abrasions result from trivial injuries and foreign bodies. Certain eye conditions like misdirected eyelashes (trichiasis) and granular deposits (concretions) on the under-surface of the eyelids can also scratch the cornea with every blink.
The following eye conditions predispose the eye to a corneal ulcer:
- Dryness of the eye (xerosis/xerophthalmia – commonly due to vitamin A deficiency)
- Inability to close the eye due to facial palsy
- Decrease/loss of normal sensations of the cornea (e.g., due to herpes or neuroparalytic keratitis)
- Waterlogging of the cornea (corneal oedema)
- Virulent bacteria like gonococcus or diphtheria bacilli invading the intact surface cells of the cornea
- Use of steroid eye drops
- Intake of immunosuppressant / steroid drugs
- Obstruction to the tear outflow channels (chronic dacryocystitis)
A corneal ulcer is an emergency situation. If you develop severe pain, redness, inability to tolerate light (photophobia), or watering/ discharge, consult your eye specialist urgently for immediate and effective treatment. Serious complications such as scarring and corneal opacity can occur, which can cause partial or total blindness.
How to prevent corneal ulcers
- Avoid scratches and abrasions in the eye. Do not let dirt or dust into the eye and, if it gets into the eyes, do not rub. Wash the eyes with plenty of clean water. If irritation persists, consult your eye doctor immediately.
- If you wear contact lenses, follow your doctor’s instructions. If pain and redness occur while wearing contact lenses, see your doctor to rule out a corneal ulcer.
- If you are a farmer, avoid getting vegetative foreign bodies into your eyes (leaves of sugar cane, maize, etc.). Such foreign bodies may be harbouring fungus. Fungal ulcers are difficult to heal. Whenever possible, wear protective (safety) glasses in windy or dusty conditions.
- If you have dry eyes (xerosis, etc.), use lubricant eye drops and oral Vitamin A as advised by your doctor.
- If you have facial palsy, the affected eye should be closed with tape at night as instructed by a doctor. People with facial palsy are prone to getting ulcers as the cornea becomes dry due to the inability of the eye to close (exposure keratitis).
- Correct misdirected lashes by surgery or get them pulled out by a doctor to avoid injury to the cornea.
- Treat the underlying diseases of the eye.
- If you have an ulcer, do not use steroid eye drops. Also try to avoid the intake of steroid and immunosuppressant drugs.
Watching television can strain the eyes. If you like to watch television, remember the following:
- Sit at least three meters (eight to ten feet) away from the television set.
- Have some extra light in the viewing room, so the room is not pitch dark.
- Make sure light is not reflected off the screen into your eyes.
- Avoid watching a television screen that is blurred, flecked or vibrating (shaking).
- Rest your eyes from time to time while watching television programmes. For example, get up and walk out of the room and do something else, like make a cup of tea.
The human vision system is not designed for long hours of computer viewing. The use of computers is growing exponentially. The amount of time one spends looking at a computer screen is also increasing. While computers enable us to be more efficient and more productive, this comes at a price – computer vision syndrome (CVS). CVS is a complex of eye and vision problems that are experienced during, and related to, computer use, and is a repetitive strain disorder. All computer-related eye problems are preventable and correctable.
Typical symptoms of CVS
- Eye strain
- Blurred vision
- Dizziness or nausea
- Headaches
- Red, dry or burning eyes
- Increase in nearsightedness
- Change in colour perception
- Slow refocusing
- Excessive fatigue
- Neck, shoulder and back pain
- Occasional double vision
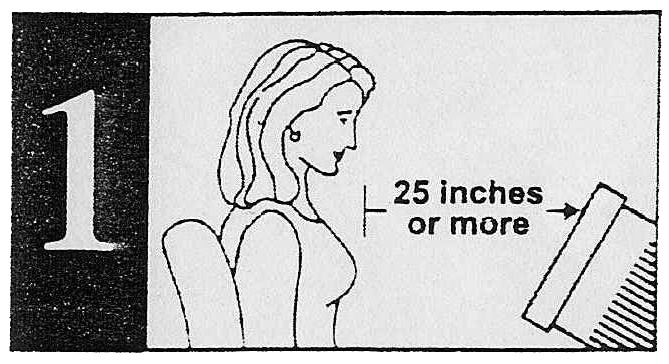
Screen distance: At least 25 inches.
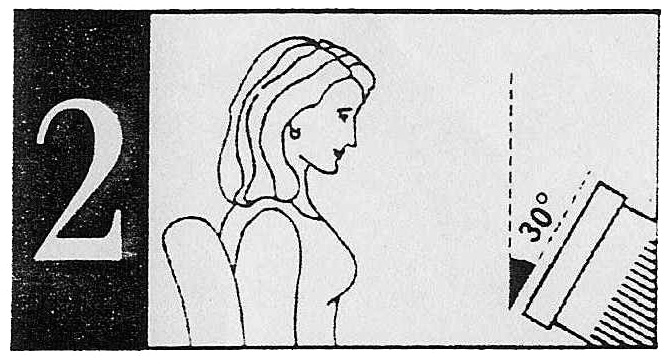
Monitor tilt: Keep monitor top slightly
farther from eyes than its bottom.
Screen: Dark letters on a light background.
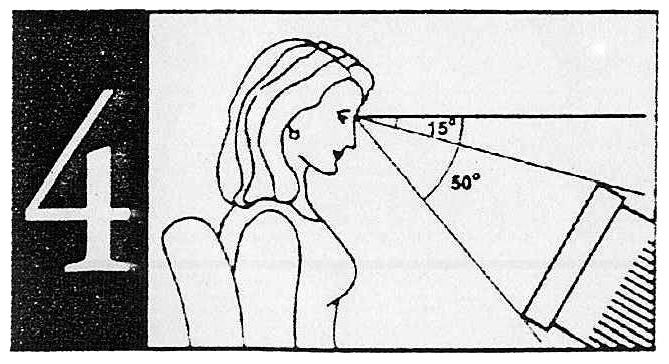
Vertical location: Viewing area of monitor 15°- 50° below horizontal eye level.
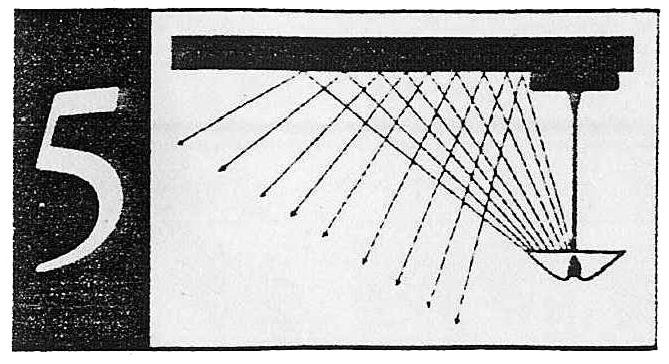
Lighting: Ceiling suspended indirect lighting. Use blinds, shades and curtains to avoid outside light and reflection.
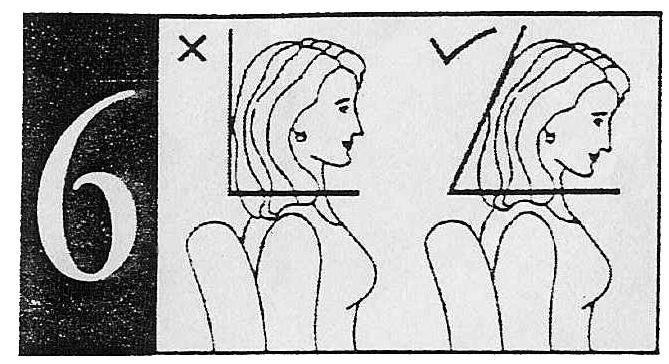
Neck posture: Use chair with arms. Flexion (head-tilt pose) causes less fatigue.
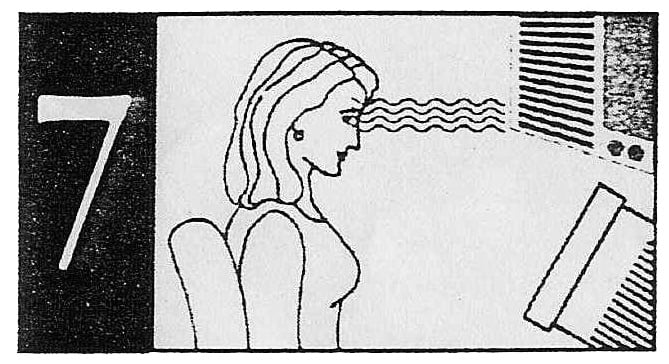
AC airflow: Avoid direct flow/draft of air on your eyes.
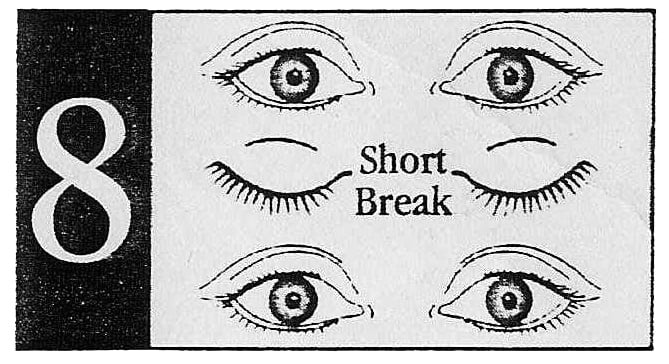
Break: Short visual break every 20 minutes.
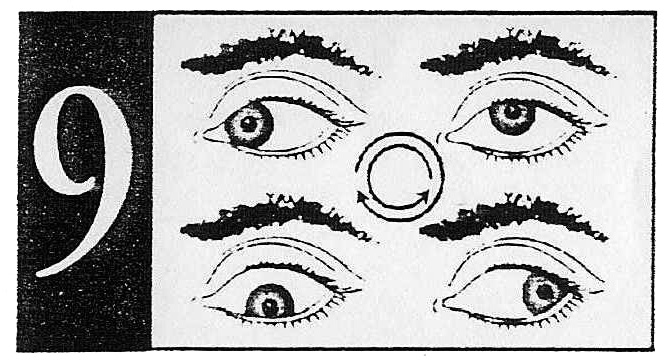
Exercise: Blink eyes a few times. Close eyelids; roll eyes behind closed eyelids clockwise, then anti-clockwise. Take a deep breath; open eyes while releasing breath.
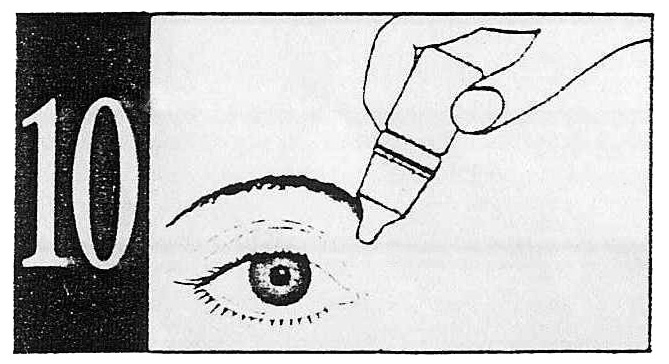
Lubricate eyes: As advised by your doctor.
Eye problems of middle age
Diabetes and high blood pressureDiabetes is a disease in which the amount of sugar in the blood is not properly controlled. It is caused by too little insulin, the hormone that is made by the pancreas and controls sugar levels in the blood. Diabetes affects all organs of the body including the eyes.
Warning! Diabetes can lead to blindness, most commonly because of damage to the blood vessels in the retina (the membrane lining the inside of the eye). In diabetic patients, additional risk factors to the eyes are pregnancy, smoking, obesity and high cholesterol levels in the blood.
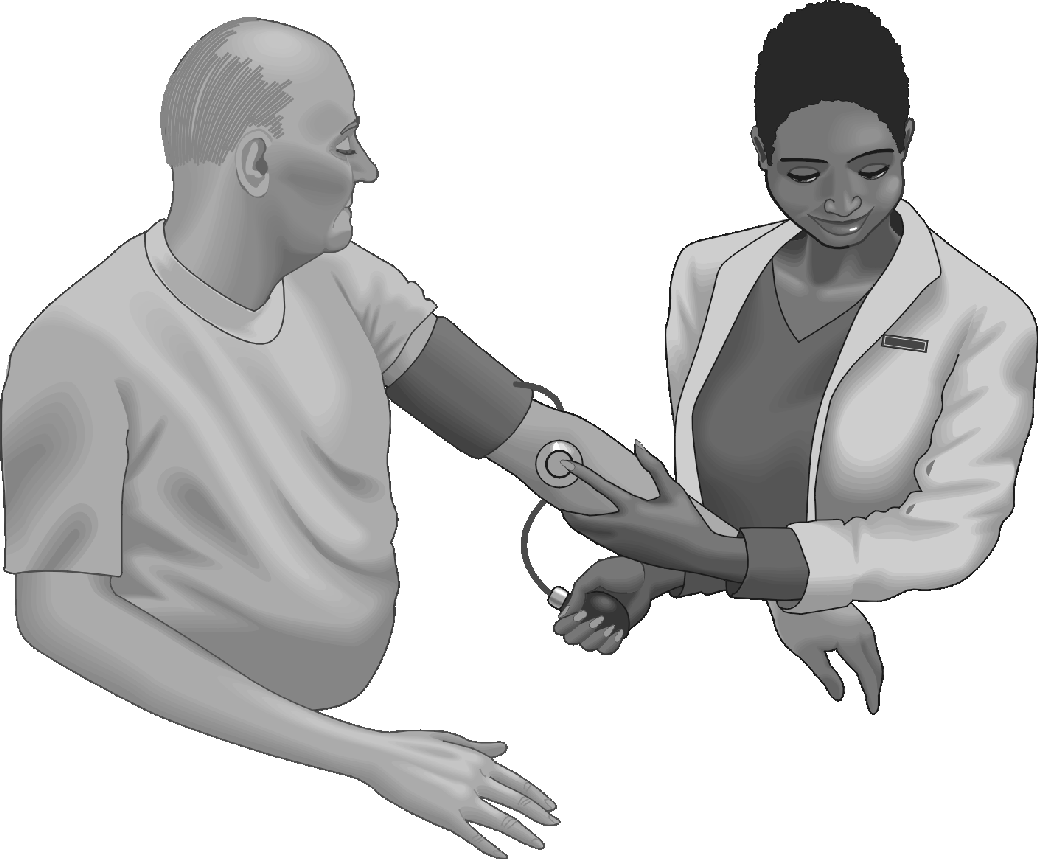 Get your blood pressure checked yearly. There are usually no warning signs for high blood pressure, although the risk increases if you gain weight as you get older.
Get your blood pressure checked yearly. There are usually no warning signs for high blood pressure, although the risk increases if you gain weight as you get older.
Warning! If you have diabetes and high blood pressure, you are at a much higher risk of eye disease than people with just one of these problems. Work hard to keep them under control with your doctor’s help. This will help you keep your eyesight in good condition.
In addition to the control of blood pressure and diabetes, fundus examination (internal examination of the dilated pupil after appropriate eyedrops) by an eye specialist is essential. See pages 92 – 107 for more information about diabetes.
Glaucoma (kala motia)Glaucoma, commonly known as kala motia, is a blinding disorder. The vision loss that occurs in this condition is irreversible. Glaucoma includes a group of eye conditions which lead to gradual damage of the nerve that takes visual impulses to the brain (optic nerve). The condition usually affects both eyes.
The nerve damage is responsible for causing blindness in such people due either to high pressure inside the eye or to impaired blood circulation to the nerve. This may happen even in eyes with normal pressure. The nerve damage causes a reduction in the field of vision, and may eventually result in complete blindness.
Glaucoma is mostly a silent killer of vision. Most often the condition is painless and, by the time one is aware of it, harm to the vision may have already occurred. Vision, once lost, cannot be regained by any medical/surgical or laser treatment. However, once detected, the progress can be halted or slowed by any of the above-mentioned treatments and further loss of vision can often be prevented.
Disciplined and regular treatment as advised by the eye physician is required so that the existing vision can be preserved. The treatment required may have to be continued for the rest of one’s life because glaucoma cannot be cured. It can only be kept in check.
Some people are at high risk of glaucoma, such as those:
- Having a relative with glaucoma
- Wearing high minus-numbered glasses (near-sightedness)
- Suffering from diabetes, hypertension or thyroid diseases
- Using steroids (eye drops, ointment or tablets)
- Who need frequent changes of eyeglass prescriptions
- Having poor night vision
- Who are detected to have high pressure in the eye
The risk increases with age. All adults should have regular eye check-ups to rule out glaucoma. Early detection of glaucoma and regular treatment will help to prevent blindness.
There is a kind of glaucoma that can happen quickly (acute angle closure glaucoma). Since it is a sight-threatening and emergency situation, seek medical help as soon as possible if you have one of the following. Note that both eyes will require treatment:
- Very bad pain in one eye
- A red or bloodshot eye
- Visions of coloured rings around lights (bulbs or candles)
- Sudden diminution of vision
- Nausea or vomiting
- High plus-numbered glasses (far-sightedness)
Glaucoma usually affects older people but can also affect newborn babies and infants. This is called ‘congenital glaucoma’ and must be treated as early as possible to prevent blindness. If your child has unusually large eyes, beware: it may be congenital glaucoma. Take him/her to an eye specialist.
Remember that you must play your part in maintaining your vision.
The hallmark of early glaucoma management:
Ensure early detection!
That means having regular eye exams.
Eye problems of old age
‘Cataract’ means any cloudiness in the lens of the eye. This cloudiness gets in the way of light entering into the eye and so it makes vision worse. It usually occurs above the age of fifty years and is commonly seen in older people when it is also called ‘senile cataract’. The causes of senile cataract are not entirely clear. A cataract can also be present at birth (congenital cataract). It can also grow at a very young age (developmental cataract).
Causes commonly linked to cataracts are:
- Age (senile cataract)
- Eye injuries
- Not enough green vegetables
- Bright sunlight (ultra-violet rays)
- Certain eye diseases
- General diseases (like diabetes, thyroid and parathyroid disorders)
- Steroids
- Gradual painless reduction of vision
- More light is required to see clearly
- Frequent change of prescriptions
- Coloured rings around light
- Improvement in near vision, i.e., one starts seeing clearly without near glasses
- Objects visible as two or more than two, e.g., one moon may be visible as many moons
- Difficulty in driving at night
- Greyish or white pupils
There is no medical cure for cataract. Cataracts can only be cured by surgically removing the clouded lens and replacing it with a small artificial lens (intra-ocular lens or IOL) to restore vision.
- You do not have to wait for the cataract to be fully mature (i.e., to wait for complete loss of vision). Rather if your quality of life is being hampered due to a decrease in vision, the surgery can be performed in the early stages of development.
- Waiting for a cataract to mature may be harmful as the chances of developing glaucoma (kala motia) are greater.
- You do not need to stay in the hospital for long. You may be sent home on the same day.
- You do not have to wait for a particular season.
- There is no laser cataract cure. Instead, a new technique of cataract removal called phacoemulsification allows cataract removal in an emulsified form through a very small cut, where a stitch is usually not required. The advantage of this technique is early rehabilitation, however, it is more expensive.
- There are less expensive techniques. Commonly used are ECCE/ IOL or MSICS/IOL (manual small incision cataract surgery with IOL). They give equally good final visual recovery.
Age-related macular degeneration is a slowly progressing, blinding disease, due to progressive damage to the macula. The macula is the central part of the retina (the innermost light sensitive layer of the eyeball) that allows us to see the fine details and appropriate colours of an object. It affects both eyes. It is a leading cause of blindness in developed countries in the population above the age of sixty-five years. In India, blindness due to ARMD has also become significant due to the increase in life span and thus an increase in the number of the aged population.
ARMD is of two types:- Dry armd: This is more common than the wet form of the disease and accounts for 90% of all ARMD cases. It is caused by the aging and thinning of the tissues of the macula. Vision loss is usually gradual and may take years. There is no effective treatment available. Low vision aids may help the patient to do reading and near vision work.
- Wet ARMD: This is less common but more severe than the dry form. It accounts for approximately 10% of all ARMD cases but causes 90% of the cases of profound blindness with ARMD. There is abnormal development of new blood vessels (choroidal neovascularisation, CNV) beneath the retinal pigment layer of the retina (RPE). The vessels can bleed and eventually cause macular scarring, which can result in a profound loss of central vision (disciform scar). It is therefore associated with comparatively rapidly progressive marked loss of vision. Fundus fluorescein angiography (FFA) helps in detecting CNV.
- Age: If you are above the age of sixty-five years, the risk of having ARMD greatly increases.
- Family history: It may run in families.
- Sex: It affects women more than men.
- Demography: It is more common in northern Europe.
- Smoking: The only environmental exposure clearly associated with macular degeneration is tobacco smoking. It is more common in smokers.
- Hypertension, heart problems, high cholesterol in blood, obesity, and high fat intake are among other possible risk factors.
- You develop difficulty in reading and close work. Words on a page look blurred.
- Colours look dim.
- Straight lines look distorted, especially at the centre of vision.
- There is alteration in the size of an object.
- A dark or empty area appears in the centre of vision.
Antioxidants: In early stages of ARMD, some specific antioxidants may help to slow down the progression of degeneration, so eat green leafy vegetables throughout your life.
Laser: May help in selected cases of wet ARMD. The vision lost cannot be regained with a laser. Low vision devices may be helpful in advanced stages of ARMD.
Photodynamic therapy (PDT) and transpupillary thermo-therapy TTT) are other newer techniques.
The aim of the treatment is to stabilize the existing vision.
Do’s of eye care- Use clean water when washing your face and eyes.
- Use protective (safety) glasses when drilling, welding, using cutting machinery, or working in dusty environments.
- Eat green vegetables, carrots, and fruits like papaya and mangoes.
- Read in proper light and in a proper sitting posture. While reading, the book should be on the table and light should:
- Come from the left and front for a right-handed person.
- Come from the right and front for a left-handed person.
- Take your child to see an eye doctor if he or she child has a squint (crossed eyes) or lazy eyes.
- Breastfeed infants if possible to avoid nutritional blindness.
- Protect your eyes when playing sports like cricket and boxing.
- Get your eyes checked every year if you are over 35 years or if you drive for a living.
- Get your children’s eyes checked before they start school and at least once or twice during their school years.
- Always see a doctor if you have blurred vision, see coloured rings around lights, have problems seeing in the dark, or have recurring pain in one or both eyes.
- Get glasses prescribed by an eye specialist and not by an optician.If you are nearing forty years of age and have difficulty reading, you may need glasses to help with far-sightedness.
- Don’t use towels and handkerchiefs used by others.
- Don’t apply kajal or surma to children with the same rod.
- Don’t let your children play with sharp objects, air guns, firecrackers, etc. Avoid games like bows and arrows and gullidanda.
- Don’t look at the sun directly, particularly during a solar eclipse.
- Don’t rub the eye if something falls into it. Rather, rinse the eye with clean water. Get medical help if the dirt or object is not washed out.
- Don’t go to quacks (people who say they know cures, but have no medical training), as their medicines may be harmful and injurious.
- Don’t decide on your own about eye-drops or medicines.
- Don’t read in dim light.
- Don’t delay the treatment of squint, red eye, any problem needing spectacles, glaucoma, cataract and injury to the eye.
- Don’t use another person’s spectacles.
Pledge eye donations during your lifetime.
Contact your local eye bank for more information.
For more information, see pages 145 – 147 of this booklet.